A New Pathogen Pressure Adding to the Coronavirus Pandemic Burden in Healthcare Facilities Around the World – Airborne Fungal Infections
Hospital-acquired fungal infections can be very dangerous and even deadly for patients who are immunocompromised or for people who have recently undergone invasive medical procedures. With concern growing within the medical profession, it is paramount that measures are taken to minimise the risk of patients falling ill from these airborne infections.
Dr Rhys Thomas, Chief Medical & Scientific Officer at PP-L says “Mould is present in all environments, not just those older facilities with inherent mould issues. Therefore, without specialist interventions, there will always be a risk of fungal infections within healthcare settings. Ensuring that the air contains extremely low levels of airborne particles/contaminants, including mould spores, will help to control the risk significantly. This is already achieved in pharmaceutical cleanrooms, where a sterile environment is created through the use of a high levels of air changes and filtration.”
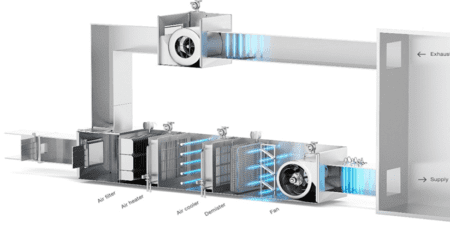
“The concentration of mould in the air may be increased due to a number of sources, such as construction, maintenance and renovation, water damage, high humidity and inadequate heating-ventilation-air conditioning (HVAC) systems. HVAC systems could become a dangerous source of mould spores if they are not well maintained, for example if mould is left to grow within the system, especially on the coils or filters as a bio-film or if mould spores from outside air are allowed to flow to the inside air.”
“The problem often gets back to inadequate ventilation systems and rate of new clean uncontaminated outside air. Previous pandemics and indeed, CDC and WHO guidance points to ventilation as a key aspect of infection prevention.”
“The minimum rate should be no less than 10 Air Changes per Hour (10ACH) or equivalent decontamination that 10 new air changes would bring in an hour if one want to control or eliminate risks within clinical settings. SARS and TB outbreaks have been quashed at this level. If one wants to deploy CO2 meters to check, this is a very easy and cost-effective method to indicate adequate ventilation, if undertaken properly in fully occupied spaces. Regular levels of 500-600ppm would indicate adequate ventilation for fully occupied spaces but it is always worth getting a qualified Engineer to interpret and review the environmental risks and systems.”
“This is where a special type of UV-C light can help; also known as Germicidal Ultraviolet light or GUV, it is a type of ultraviolet light that can disinfect air. Importantly, as well as removing harmful bacteria and viruses, it can also inactivate/kill mould spores.”
“GUV devices, when specified for the right environmental conditions and target microbe range, can be installed safely out of sight within HVAC ductwork, killing the mould spores in the air flow before they enter the room. These in-duct devices can also kill the moulds growing on the moist interiors of the HVAC system such as the cooling coils, filters, insulation and duct surfaces.”
“Inside the hospital rooms, A US study1 found that germicidal UV lamps fitted in a building’s HVAC system led to a dramatic decrease in airborne fungal spores, with total concentrations reducing from a baseline 239.52 (102 CFU/m3) to just 2.98 (102 CFU/m3). This represents a decrease of 98.8% from baseline levels.”
“The UV-C lamps also killed fungal spores on the interior surfaces of the HVAC system. Concentrations of fungi were tested on samples of the insulation taken from the air handling unit. Total fungi concentrations reduced from a baseline 2240.55 (103 CFU/m2) to just 30.51 (103 CFU/m2), representing a decrease of 98.6%.”
UV-C can also be utilised within GUV upper-room emitters or in portable medical grade air purification devices. With proper specification, these units can also disinfect the air and reduce the concentration of mould spores where it is not possible or practicable to retro-fit devices into existing HVAC systems.
GUV is microbe and variant-agnostic, so can also be used to help control other airborne infections including COVID-19 and Influenza A. SARS-CoV-2 is a straightforward, simple, single-strand RNA virus, and it doesn’t take very much UV light energy or exposure time to destroy it.
Dr Thomas added, “UV-C has been deployed in healthcare settings for decades. During the first SARS pandemic in 2002/2003, our products were used in three major installations in Hong Kong and Singapore’s hospitals. HVAC germicidal UV devices were engineered, selected and installed into the duct systems of hospitals, in order to create a safer environment. Infection control was also implemented locally directly at source of infection, above patient beds in the wards, to intercept and inactivate anything that may have been in the exhaled breath of patients.”
“These hospitals were then fully equipped with the necessary tools to deal with airborne viruses and bacteria. This dual infection prevention approach of the ‘total building system’ and ‘local source control’ engineering solutions within the hospitals proved highly effective because infection was quashed.”
“With the risk of COVID-19 transmission within healthcare settings in the UK still substantial, along with the mounting issues with airborne fungal infections and re-emerging concerns about other respiratory viruses such as Influenza rising over the winter, these correctly engineered ventilation and GUV engineered solutions could offer hospitals a crucial, and even life-saving weapon to their armoury.”
“By making use of the powers of Germicidal UV, healthcare settings around the world can prevent and control the spread of harmful fungal, and other dangerous pathogens.”
Summary
- Reduce the risk of fungal infections by ensuring that the air contains extremely low levels of airborne contaminants, including viruses, bacteria and mould spores using correctly engineered, safe, germicidal ultraviolet air disinfection (GUV).
- The concentration of mould in the air may be high due construction/maintenance
- activities; water contamination; high humidity and inadequate ventilation systems.
- Improving with HEPA Filters alone is not often not practicable or effective.
- Ventilation in clinical settings should be no less than 10 clean outside air changes per hour or equivalent air decontamination rate using GUV to compensate.
- Inadequate ventilation can be identified with CO2 meters within occupied spaces. One should be observing less than 600ppm CO2 as an indicator of adequate ventilation.
- GUV can be used within ventilation systems, or as traditional GUV upper-room emitters and in medical grade air purification devices. These devices can disinfect air by removing harmful mould spores, bacteria and viruses.
- The above are recommended by the CDC, and regulators and institutions globally to help eliminate and prevent harm from pathogens, including SARS-CoV-2.
References
1http://journals.asm.org/doi/full/10.1128/AEM.67.8.3712-3715.2001
http://www.tandfonline.com/doi/full/10.1080/15459620600909799
http://iris.uniroma1.it/retrieve/handle/11573/1449807/1582402/DOrazio_Air-bio-contamination_2020.pdf http://www.sciencedirect.com/science/article/pii/S0196655317312531




Leave a Reply